MD Program Overview
Our four-year MD program is community informed and evidence-based to align with the School of Medicine’s social accountability mandate. It is rooted in principles of community-driven care and cultural respect and safety, with Equity, Diversity and Inclusion (EDI), intentionally embedded across all aspects of the program. It has been purposely constructed to align with our vision, mission, values, program objectives and learning outcomes.
In order to best support students’ development of problem-solving skills and meaning-making, we follow the principles of a model known as the Master Adaptive Learner characterized by inquiry-based learning, small group case-based learning, and purposeful revisiting of concepts. Team projects, team-based learning and service learning provide opportunities to learn with health partners in the community. The aim is to produce physicians who are not only clinically competent but also equipped to advocate for and lead change within the healthcare profession.
Explore MD Program
We aim to prepare graduates who:
- Are clinically competent and compassionate physicians who act with the highest standards of professionalism and ethical practice to meet the healthcare needs of all, including the unique needs, health practices and traditional care models of Indigenous, Black, and other equity-deserving and medically underserved populations.
- Embrace generalism as a key pillar to all clinical learning and graduates’ practice as a means to prioritize primary care as a career choice.
- Advocate for health systems transformation and social justice and address the social determinants of health, with an understanding of health systems and exclusionary systemic barriers at an individual, institutional and population level.
- Are trained in cultural safety, anti-racism, anti-oppression, trauma and violence-informed approaches, social justice, and rights-based approaches to health to better serve patients, families and communities as co-creators, allies and advocates.
- Work collaboratively with patients, families and communities by providing high-quality, person-centred care through meaningful and integrated clinical training in interprofessional community settings.
- Apply leading technological practices in medicine ethically with a focus on improving quality of care and patient outcomes.
- Address the unique needs of an aging population to support aging with dignity in the community, provide holistic care, promote health and well-being, and deliver mental health services at a primary care level.
- Possess the knowledge and skills to improve the environmental sustainability of health systems and to advocate for and address the interconnected impact of climate change on the health of patients, families, communities, health systems and the planet.
- Understand and reflect on the unique histories and current contexts for Indigenous health and demonstrate a commitment to Reconciliation and decolonization of health systems through cultural humility and ongoing reflection in their practice, as well as through ongoing, reciprocal partnerships and a continuous process of co-creation with Indigenous communities.
We aim to promote a learning environment that will:
- Foster critical thinking, inquiry and evidence-based decisions using the latest technology and data-driven reflective practices.
- Provide meaningful and integrated teaching and learning experiences and research training in clinical, patient and community-centred settings that reflect community health needs and promote person-centred and community-based healthcare.
- Foster deep learning and support students’ professional development through a competency-based, active and experiential learning medical education model with programmatic assessments.
- Promote a culture of inclusion, humility, engagement and mutual respect.
- Foster an environment that supports the health, well-being, and resilience of students and the individuals who teach, mentor and support them.
- Encourage reflexivity, continuous growth and improvement at the personal, professional and institutional level.
We aim to establish an environment of inclusion through:
- provision of equal access to students who are underrepresented in medicine (especially students who are Indigenous, Black and from other equity-deserving backgrounds) and support their development.
- advancement of International Medical Graduates (IMGs) into clinical practice to augment physician supply and to enhance the diversity of the physician workforce.
The MD Program learning outcomes align with the CanMEDS 2015 framework as well as with the College of Family Physicians of Canada CanMEDS Family Medicine framework and the Indigenous Health Supplement Key and Enabling First Nations, Inuit and Metis Health’s core competencies.
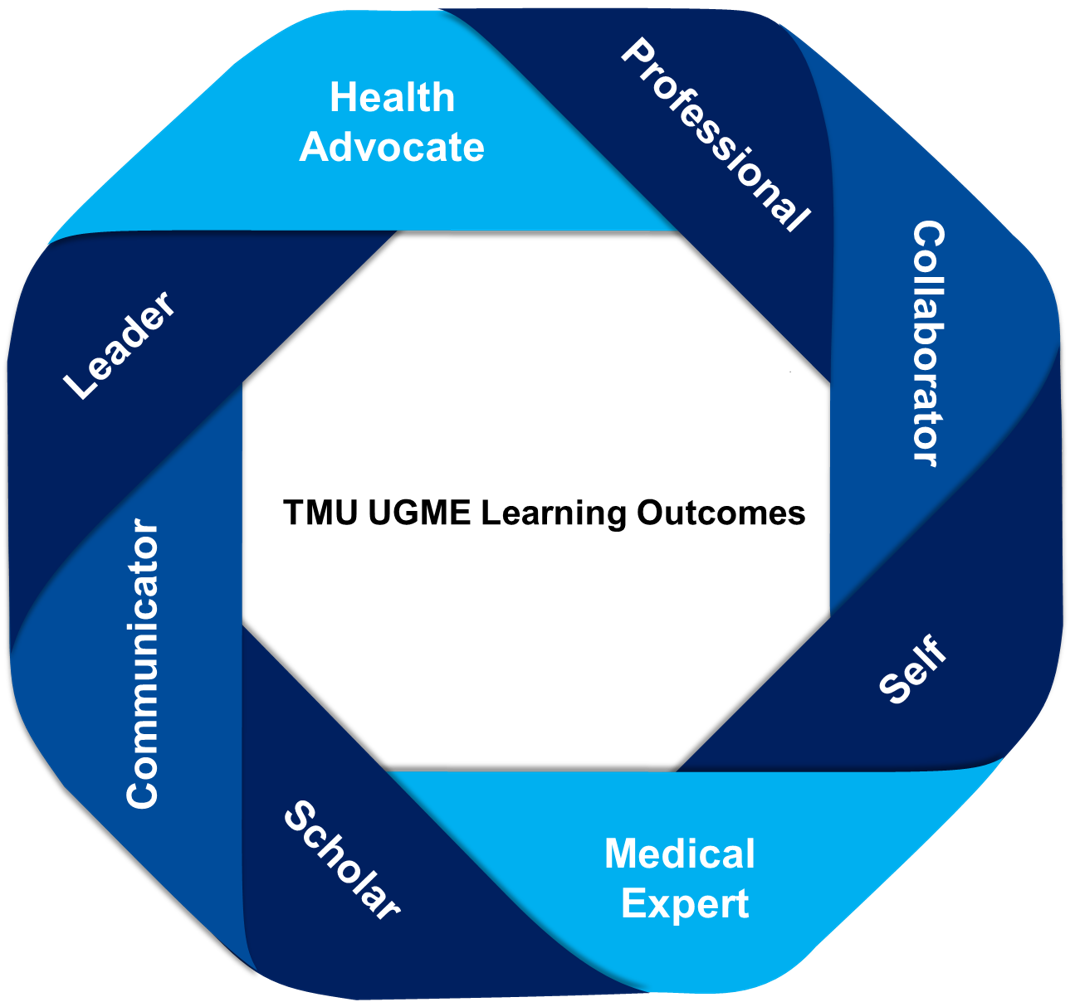
The learning outcomes of our program are grouped thematically under the following eight roles, with the expectation that a competent graduating future physician seamlessly integrates the competencies of each:
Advocacy is the ability to support and/or enable a process of change in care that improves person-centered care. A health advocate contributes with respect, from evidence, and demonstrates true humility to advocate with their patients to support enhancement of person-centred care. TMU UGME graduates will always seek to advance health equity and improve healthcare services while addressing the impacts of privilege and marginalization on health outcomes at the individual, institution, community, government and global level.
A collaborator builds and maintains mutually beneficial relationships with the patient and the broader healthcare team to deliver and improve safe, high-quality, equitable, and person-centred care to all, including diverse and equity-deserving communities. A person’s healthcare team includes the individual's self-defined care network (e.g. family, caregivers, and community), health professionals and other providers.
As health professionals, physicians are committed to values and standards of care that govern the profession while improving health and well-being for patients, colleagues, health professionals and society. As future physicians, TMU UGME students learn and demonstrate high standards (personal and as physician-learner) through ethical, equitable, anti-discriminatory, inclusion-focused action in care, involved community activities, and in their personal life. They are accountable to the standards of the medical profession, our school, university, and society.
As leaders, physicians engage with patients, families, communities, health professionals, and other partners in delivering innovations for care. Leaders facilitate change and improvement by engaging with others, reaching consensus through collaboration, and using effective communication, while balancing personal and professional roles. Leaders also ensure continuous improvement of person-centered care and health system functions while retaining strong personal, clinical, scholarly and educational roles. Physician leaders advocate as “participative leaders” for health equity at all levels of the healthcare system through culturally safe community-driven approaches.
Scholars adopt a lifelong commitment to ongoing learning to improve patient care and the profession through reflection, integration and the sharing of knowledge. Scholars contribute to expanding medical knowledge. Students, as future physicians, demonstrate ethical, socially accountable scholarship in Program learning, healthcare participation and team-based projects.
A Communicator seeks out, assesses, and shares essential information to advance equitable, inclusive, and quality person-centred healthcare for all. As communicators, students as future physicians form therapeutic relationships with patients, their families, caregivers; members of the interprofessional healthcare team, other professionals; and communities. This involves dynamic exchanges before, during, and after the medical encounter.
Medical Experts embrace and demonstrate daily all professional roles of healthcare. As evolving Medical Experts, students integrate all TMU UGME Learning Objectives, applying knowledge, skills, and professional values to understand and support high-quality equitable and accessible care to the person, and community. Key professional values include a commitment to lifelong learning and providing holistic personal care that is inclusive, equitable, anti-racist, culturally safe, and protects the rights of all. Clinical encounters require students to use a broad range of skills to participate in care for diverse patient populations across multiple communities and the lifespan.
The role of Self emphasizes the importance of continually developing each future physician as a person. While managing expectations within the practice of medicine, and in order to meet the challenges of today’s world and the future world, it is important for students to maintain wellness, a strong personal support process, resilience and humanity. This involves learning to manage their personal lives by adopting habits that foster health in mind and body for themselves and their communities of support.
The CanMEDS framework features seven roles. We have augmented this framework to reflect our program’s distinct philosophy. Medical curricula are usually driven by the Medical Expert role. Indeed, this role is placed at the centre in the pictorial that CanMEDS has created to depict the roles. However, the intended student-focused philosophy of our program’s curriculum, and the goals of the Ontario Quadruple Aim, led to the creation of an additional student outcome role.
The new role we have adopted for our MD program is titled “Self”. It is intended to convey the importance of bringing one’s authentic self, as a human being, to every facet of one’s life, including the professional aspect, while acknowledging the critical nature of supporting the development of personal wellness and success. Therefore, the articulation of learning outcomes in our proposed curriculum, which begins with the Health Advocate and Leader roles, culminates with both the Medical Expert and Self roles. The relationship of the eight roles in our curriculum is depicted in Figure 1.
Teaching and Learning Methods
An integrated approach driven by the community and emphasizing interactions with interdisciplinary faculty will be used to deliver the curriculum. The approach will also be guided by the student experience, ensuring that the active and interactive aspects of learning are emphasized. The prominent instructional methods include:
- Case-based learning
- Team-based learning, team-based simulations and projects
- Laboratory learning, clinical experiential learning and simulation
- Early clinical experiences, longitudinal experiential learning, service learning, and interprofessional clinical experiences
- Self-directed and asynchronous learning