Joshua Manansala
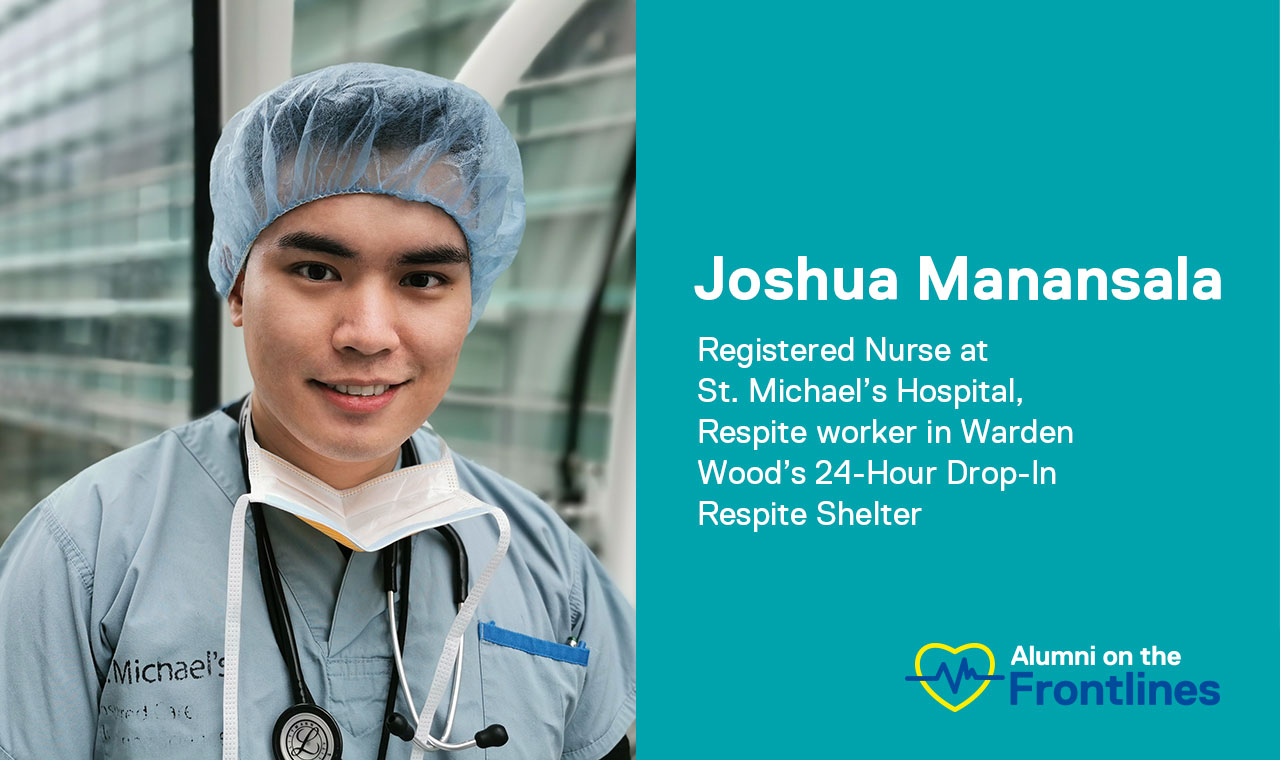
Joshua Manansala is a Registered Nurse at St. Michael’s Hospital and a respite worker at a 24-Hour Drop-In Respite Shelter in Toronto.
During the COVID-19 pandemic, healthcare professionals, food service workers, truck drivers and countless more involved in the supply chain for essential goods and services are working harder than ever and facing considerable personal risk for the good of society. In this series, we asked alumni on the frontlines of this pandemic to share their experience with us.
Joshua Manansala is a Registered Nurse at St. Michael’s Hospital. He works in different inpatient units throughout the hospital, including St. Michael’s COVID-19 Assessment Centre. As part of his role he provides direct patient care, which includes performing thorough health assessments, administering medications, participating in interdisciplinary rounds as needed, providing relevant patient and family teaching, and much more.
How has your work changed since COVID-19?
While floating in different units is the norm for me, the number of units requiring staffing needs has increased, sometimes I now work in the Emergency Department to screen for COVID. For patients with positive [test results] or suspected cases of COVID, I have to cluster my care even more to lessen my risk of exposure. Of course, this is in balance with very close patient monitoring since a patient’s health can significantly deteriorate within a matter of hours.
You have two roles — at the hospital and at the shelter?
Can you tell us more about that? How are they different?
Absolutely. I am a respite worker in Warden Wood’s 24-Hour Drop-In Respite Shelter. My role is to provide direct client service as part of a team in a non-clinical manner. While it is a non-clinical role, there are a lot of transferable skills between the positions like therapeutic communication, listening skills, de-escalation techniques, and critical thinking. Working at the shelter provides me with a mental break from being an RN, as well as an opportunity to gain perspective on how COVID affects the homeless population in our communities.
How does the experience of the mainstream public differ with respect to COVID-19 from those who are more vulnerable, such as those living in shelters?
It is very different. First, the mainstream public has the privilege of having a place to call home — they have the security and all of the privileges that come with having a house. People experiencing homelessness do not have secure and permanent housing, and this exposes them to a multitude of problems, including diseases. Traditionally, homeless shelters are crowded spaces, and with crowding, diseases like Tuberculosis and COVID spread more easily. This is why social distancing efforts must be enforced in shelters. Also, because of their situation, people experiencing homelessness do not have much control over their own social determinants of health, like having equitable access to health services, social supports, and income.
Can you tell us about something or someone that’s inspired you during this experience?
A man I met at the shelter recently got housing. His character, mood and thinking, which was complicated by a mental health condition, has changed dramatically since he received professional help in the hospital and community. Our shelter became a sanctuary for him to take time, reflect, get the services that he needed, and work with our case management team. The work that his case managers and social workers do, and how they have collaborated with health care professionals to create and follow a plan of care in the community setting is extremely important. To a larger extent, his story of success is possible because people believed in the good work that shelters do and the services that are provided. It all started because someone cared.
What do you want people to know about your experience during this time?
I want people to know that yes, being a nurse can be a very rewarding profession, but it can be physically and emotionally demanding, especially during times like this. Taking care of patients with COVID has made me realize how serious this pandemic is. We must follow all precautions strictly and hold each other accountable. Also, I want people to think of those who are more vulnerable in our society and advocate with them.
What is the biggest challenge you are facing?
In general, I would say the biggest challenge right now is keeping up morale during tough times. Since most of my family works in health care, we are afraid to bring COVID to our house. It is especially difficult to watch a patient who is deteriorating or dying who cannot have their loved ones in their room with them.
What do you think the lasting impact of COVID-19 will be to your work, and you personally?
Personally, an important lesson is to not take things (such as having a home), for granted and to be grateful. I have gained a new appreciation on the importance of building healthy communities by providing comprehensive supports and one that focuses on prevention rather than cure. This pandemic also taught me that when tough times come, we can expect a more united community, and that through any hardship we are never alone.